Prostate Cancer
Prostate cancer is the second most common cancer in Australian men. Prostate cancer is more common over the age of 65 and it rarely affects men below the age of 40. One in 7 men will be diagnosed with prostate cancer by the age of 85. It is one of the most curable cancers when detected and managed early.
Symptoms
Prostate cancer does not show any visible symptoms in its early stages. It is difficult to identify unless a person visits the doctor to get a medical checkup (PSA and physical examination)
Symptoms that may occur include:
Urinating frequently during the day
Nocturia (urinating frequently at night)
Waiting to begin urinating
Having a weak stream that starts and stops
Dribbling after finishing urinating
Poor emptying of the bladder
Urgency to get the to bathroom quickly
Pain on urination
Presence of blood in the urine
Frequent pain in the hips, pelvis or lower back
Tests
A prostate biopsy is required to confirm the diagnosis of prostate cancer before any treatment options are considered.
Prostate MRI scans can give very useful information on the anatomy of the prostate gland and any abnormal areas or lesions within the prostate. It also gives useful information on the size, location and suspiciousness of the any prostate lesions identified.
CT scans and bones scans are used to make sure the cancer has not spread to the bones or abdomen.
Types of Prostate Biopsy
TRUS biopsy. Transrectal ultrasound-guided (TRUS) prostate biopsy involves taking multiple samples of the prostate using a special needle. The surgeon uses an ultrasound probe placed in the rectum to visualise the prostate and guide these needle biopsies. These needles biopsies can be taken systematically throughout the prostate and specifically targetting any suspicious areas on ultrasound or MRI imaging. The procedure can be performed under local anaesthetic or light sedation. Despite the routine use of antibiotics, this procedure carries a 2-3% risk of severe infection and may require hospitalisation.
Transperineal prostate biopsy. Transperineal prostate biopsy also takes multiple samples of the prostate using a special needle. It differs from TRUS biopsy in that the needles pass through the area of skin in the perineum rather than through the wall of the rectum. The main advantage is that it has a minimal risk of severe infection. This technique, however, takes longer than TRUS biopsy and often requires a general anaesthetic.
MRI-ultrasound fusion biopsy. If a prostate MRI identifies any suspicious lesions within the prostate gland, these lesions can be “targetted” during TRUS or transperineal prostate biopsy.
Stages of Prostate Cancer
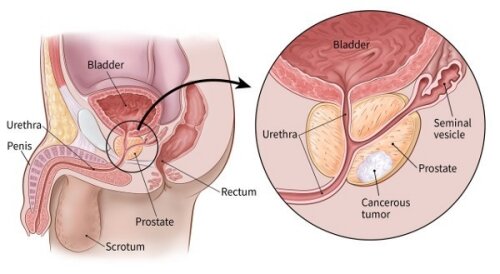
There are a number of stages in the development of prostate cancer. These stages determine how far the cancer may have spread. These stages help us to decide on the the best possible treatment plan.
Stage I: The tumor is small and invisible to the human eye. It may be seen on an imaging test. The cancer is still localized in the prostate and hasn’t spread to other areas.
Stage II: A digital rectal exam or MRI scan can be used to detect the tumour. The cancer has not moved to other areas.
Stage III: The cancer has spread locally to areas near the prostate gland such as the seminal vesicles or the pelvic lymph nodes.
Stage IV: The cancer has spread to other areas far away from the prostate gland such as the bones or other organs.
Treatment
The treatment of prostate cancer depends on a number of factors including:
Individual patient factors (such as age and overall health)
Prostate-Specific Antigen (PSA) levels
Tumor aggressiveness (Grade Group or Gleason Score)
Spread of the tumor (Prostate Cancer Stage)
Treatments for prostate cancer include:
Active surveillance. Regular monitoring of slow-growing prostate cancers where it is not life threatening, without any active treatment.
Focal therapy. Using various types of energy sources to ablate the cancer lesion and preserve the rest of the prostate gland.
Robotic Surgery. Robotic radical prostatectomy is a minimally invasive procedure to remove the entire prostate gland and the seminal vesicles. At Adelaide Urology Care, we also performed a meticulous removal of lymph nodes in the pelvis which are the first areas that prostate cancer can microscopically spread to (robotic pelvic lymph node dissection). In localised prostate cancer, the goal of this procedure is a cancer cure. In high-risk or locally advanced prostate cancer, radical prostatectomy can be used in combination with radiotherapy and hormone treatment (an approach called multimodal therapy). This approach aims to maximise cancer control and delay the time to disease progression or recurrence.
Salvage prostatectomy. Salvage prostatectomy is undertaken when prior treatments to control localised prostate cancer have failed and cancer has come back. If salvage prostatectomy is performed, the risks of urinary incontinence and erectile dysfunction are much higher particularly if performed after prior radiotherapy
Radiation therapy. Using X-rays to destroy cancer cells.
Hormone treatment. Injections to reduce testosterone, which can help slow the growth of cancer.
Chemotherapy. May be offered in advanced prostate cancer if cancer has spread to other organs.
Contact
At Adelaide Urology Care, we are committed to giving you the personalised care you need. Please do not hesitate to contact us for more information.
Male Reproductive Tract
Prostate Cancer Diagram
Online Enquiry Form
Prostate MRI Scan
More Information
Reliable and up-to-date health information is important for understanding and managing your health. A list of trustworthy and reputable medical websites is provided below. Please click on the links for further useful information on Prostate Cancer.
Prostate Cancer Foundation of Australia - Localised Prostate Cancer
Prostate Cancer Foundation of Australia - Advanced Prostate Cancer
Prostate Cancer Foundation of Australia - Younger Men (≤ 50 years)
National Comprehensive Cancer Center Guidelines for Patients
European Association of Urology Patient Portal - Prostate Cancer